Abstract
Background: Vaso-occlusive crises (VOCs) are the hallmark of sickle cell disease (SCD) and are associated with significant morbidity and mortality. Crizanlizumab, a first-in-class humanized anti-P-selectin IgG2 mAb, is approved in >40 countries to reduce/prevent VOCs in SCD patients aged ≥16 yrs. Inclacumab, a fully human anti-P-selectin IgG4 mAb, is in clinical development for SCD. In vitro data suggest that inclacumab may show stronger affinity to P-selectin and greater maximal inhibition of cell-cell interactions vs crizanlizumab (Geng et al ASH 2020).
Aim: We investigated in blinded experiments whether crizanlizumab and inclacumab can be differentiated in terms of P-selectin binding and inhibition of P-selectin-mediated cell-cell interactions, via 5 different in vitro assays, including testing of blood samples from healthy volunteers and SCD patients.
Methods: For both mAbs, we assessed: P-selectin affinity (surface plasmon resonance [SPR]/Biacore assay); inhibition of adhesion of P-selectin-expressing cells to P-selectin glycoprotein ligand-1 (PSGL-1; cell adhesion bioassay); inhibition of platelet aggregation in native blood from healthy volunteers (whole blood impedance aggregometry [WBA] and flow cytometry-based platelet-leukocyte aggregate [PLA] assays); and inhibition of adhesion of SCD patient whole blood or isolated leukocytes to P-selectin-coated substrate under physiologically relevant shear rates in microfluidic systems (flow adhesion bioassays).
Results: The SPR/Biacore assay indicated that both mAbs recognize P-selectin with binding affinities of the same order of magnitude, although there was a trend towards higher binding affinity with inclacumab (mean equilibrium dissociation constant [K D ± standard deviation]: 12.4 ± 1.0 nM [crizanlizumab] vs 6.7 ± 0.7 nM [inclacumab]). However, the function-related cell adhesion bioassay revealed a significant difference between the mAbs in their ability to inhibit adhesion of P-selectin-expressing cells to PSGL-1. Crizanlizumab showed stronger inhibition than inclacumab (potency vs crizanlizumab reference standard: 98.0% for the crizanlizumab control sample [95% CI 85.2‒112.7%] and 26.2% for the inclacumab sample [95% CI 20.7%‒32.6%]).
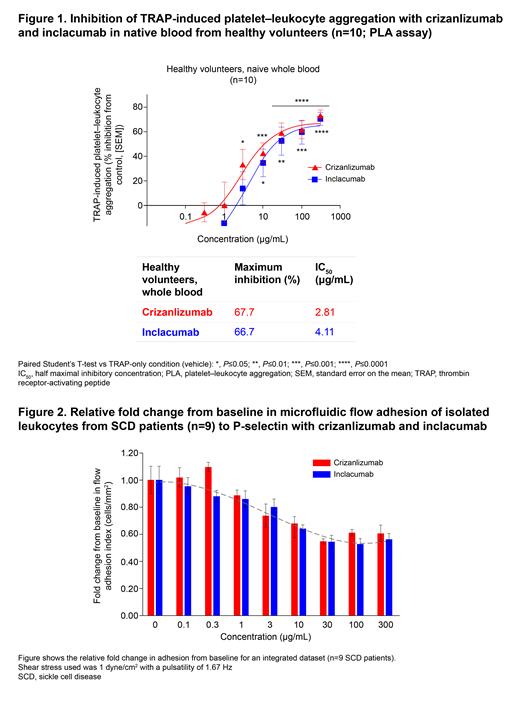
Native whole blood samples for WBA and PLA assays were provided by 12 and 10 healthy volunteers, respectively. Blocking of platelet (WBA assay) or platelet-leukocyte aggregation (PLA assay) in whole blood was comparable for crizanlizumab and inclacumab, with a clear trend towards stronger inhibition by crizanlizumab. In the WBA assay, the half maximal inhibitory concentration (IC 50) was twice as high with inclacumab (10.36 μg/mL) as crizanlizumab (5.11 μg/mL); similar data were seen in the PLA assay (Figure 1; IC 50: 4.11 vs 2.81 μg/mL for inclacumab vs crizanlizumab).
Blood samples were provided by 9 SCD patients for the flow adhesion bioassays. Dose-dependent inhibition of adhesion of whole blood and isolated leukocytes to P-selectin was seen with both crizanlizumab and inclacumab, with no difference observed between them (Figure 2). A mAb concentration of 10 μg/mL resulted in statistically significant inhibition of adhesion by 60‒75%; further increasing the mAb concentration did not result in stronger inhibition of adhesion beyond this threshold. In relation to the clinically approved crizanlizumab dose (5.0 mg/kg), a concentration of 100 μg/mL corresponds with the maximum plasma concentration (C max) and ~10-15 μg/mL corresponds with the trough concentration (C trough).
Conclusions: While the SPR/Biacore data suggested higher P-selectin binding affinity for inclacumab compared with crizanlizumab, there was a stronger inhibition of P-selectin-mediated cell adhesion with crizanlizumab vs inclacumab in other well-characterized functional in vitro assays. In microfluidic flow adhesion bioassays, blockage of cell adhesion from SCD whole blood and leukocytes was comparable for both mAbs. In summary, these data indicate that comparable or stronger blockage of cell adhesion with crizanlizumab vs inclacumab does not require superior P-selectin binding affinity. The data from healthy volunteers will be complemented by data from SCD patients for the WBA and PLA assays. Ultimately, clinical data are required to evaluate potential differences in the profiles and efficacy of crizanlizumab and inclacumab as treatments for SCD patients.
Rubic-Schneider: Novartis Pharma AG: Current Employment. Sundd: CSL Behring Inc: Research Funding; Bayer: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding. Ledieu: Novartis Pharma AG: Current Employment, Current holder of stock options in a privately-held company. Garcia: Novartis Pharma AG: Current Employment. Hehlen: Novartis Pharma AG: Current Employment. Burnet-Merlin: Light Chain Bioscience - Novimmune SA: Current Employment; Novartis Pharma AG: Ended employment in the past 24 months. Cochin de Billy: Novartis Pharma AG: Current Employment. Greutmann: Novartis Pharma AG: Current Employment, Current holder of individual stocks in a privately-held company, Current holder of stock options in a privately-held company. Krӧner: Novartis Pharma AG: Current Employment, Current equity holder in publicly-traded company, Patents & Royalties: WO2021087050A1. Verneret: Novartis Pharma AG: Current Employment, Current holder of stock options in a privately-held company. Bruederle: Novartis Pharma AG: Current Employment. Gao: Functional Fluidics: Current Employment. Dajee: Novartis: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal